Importance of Optimal Metabolic Health in Your Overall Well-being
Metabolic health plays a crucial role in overall well-being as it directly affects various aspects of physical and mental health. Metabolism refers to the complex set of chemical reactions that occur within the body to convert the food eaten into energy.
When you're metabolically healthy, it supports the proper functioning of body systems and contributes to overall health and vitality. Here are some reasons why optimal metabolic health is important for overall well-being:
Energy production – Optimal metabolic health ensures efficient energy production. When metabolism is functioning optimally, it efficiently converts the nutrients from food into energy that the body needs to carry out daily activities. This energy is essential for physical performance, mental focus, and overall productivity.
Weight management – A healthy metabolism helps regulate body fat and maintenence of a healthy weight. When the metabolism is balanced, it effectively processes and utilizes calories, preventing excessive weight gain. Conversely, poor metabolic health can lead to weight gain, burning fewer calories, and obesity, increasing the risk of various health conditions such as diabetes, heart disease, and certain cancers.
Blood sugar regulation – Proper metabolic function helps regulate blood sugar levels. When people consume carbohydrates, the body breaks them down into glucose, which is then used as fuel. A healthy metabolism efficiently manages glucose levels, preventing spikes and crashes. On the other hand, metabolic dysfunction can lead to insulin resistance and impaired glucose regulation, increasing the risk of type 2 diabetes and heart disease.
Hormonal balance – Metabolic health influences hormonal balance. Hormones play a critical role in various bodily functions, including growth, metabolism, reproduction, and mood regulation. Imbalances in hormones, such as insulin, leptin, cortisol, and thyroid hormones can occur due to metabolic dysfunction, leading to a range of health issues, including weight gain, mood disorders, heart disease, nonalcoholic fatty liver disease and fertility problems.
Cardiovascular health – Metabolic health is closely linked to cardiovascular health. Poor metabolic function, often associated with conditions like obesity, high blood pressure, and high cholesterol, can increase the risk of heart disease, stroke, and other cardiovascular problems. Maintaining a metabolically healthy condition through lifestyle choices like a balanced diet and regular exercise helps support cardiovascular well-being.
Mental well-being – Optimal metabolic health contributes to mental well-being. Nutrient deficiencies and imbalances resulting from metabolic dysfunction can affect brain function, mood, and cognitive abilities. Additionally, chronic conditions associated with poor metabolic health, such as diabetes and obesity, have been linked to an increased risk of mental health disorders like depression and anxiety.
Understanding Insulin Resistance and Its Impact on Metabolism
Insulin resistance is a condition in which the body's cells become less responsive to the hormone insulin. Insulin is produced by the pancreas and plays a crucial role in regulating blood sugar levels by facilitating the uptake of glucose from the bloodstream into cells for energy production or storage.
In individuals with insulin resistance, cells become less sensitive to the action of insulin, leading to impaired glucose uptake.
When insulin resistance occurs, the body compensates by producing higher and higher levels of insulin to try to overcome the resistance and maintain blood sugar control. This compensatory hyperinsulinemia can contribute to several metabolic changes:
Impaired glucose regulation – As cells become less responsive to insulin, glucose uptake is reduced, resulting in elevated blood sugar levels. This can lead to prediabetes and, if left unmanaged, type 2 diabetes.
Dyslipidemia – Insulin resistance is often associated with alterations in lipid metabolism. It can lead to elevated triglyceride levels, decreased levels of high-density lipoprotein (HDL) cholesterol (the “good” cholesterol), and increased levels of small, dense low-density lipoprotein (LDL) particles (the “bad” cholesterol).
These changes can contribute to the development of atherosclerosis and cardiovascular disease.
Weight gain and obesity – Insulin resistance can promote weight gain and obesity. Insulin is involved in fat storage, and when cells are resistant to its effects, excess glucose is converted into body fat, slowing metabolism that leads to weight gain. Increased insulin levels also inhibit the breakdown of stored fat, making it harder for the body to utilize fat as an energy source.
Inflammation – Insulin resistance can contribute to chronic low-grade inflammation throughout the body. This inflammation is associated with various metabolic disorders and an increased risk of cardiovascular disease and other chronic conditions.

The Connection Between Insulin Resistance and Chronic Diseases
Insulin resistance is strongly linked to the development of several chronic diseases:
Type 2 Diabetes
Insulin resistance is a primary factor in the development of type 2 diabetes. Over time, the pancreas may struggle to produce enough insulin to compensate for the resistance, leading to chronically elevated blood sugar levels and the onset of diabetes.
Cardiovascular Disease
Insulin resistance and the associated dyslipidemia contribute to the development of heart disease. Elevated insulin levels can promote the formation of plaques in the arteries, leading to atherosclerosis, hypertension, and an increased risk of heart attacks and strokes.
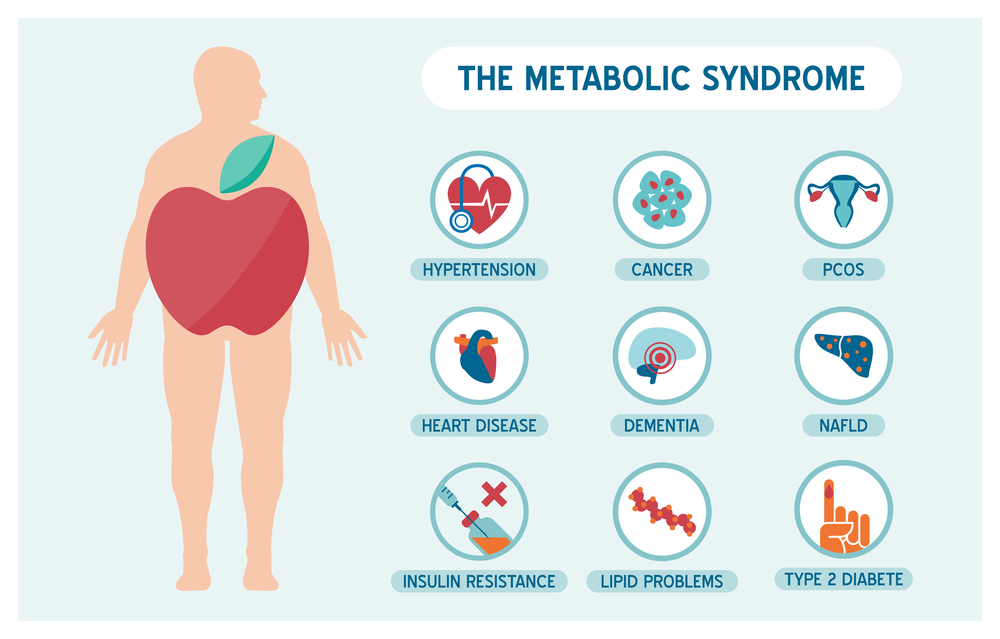
Metabolic Syndrome
Metabolic syndrome is a serious condition that afflicts millions of people and puts them at risk of fatal consequences. Insulin resistance is a central feature of metabolic syndrome, a cluster of conditions that include abdominal obesity, high blood pressure, high triglyceride levels, low HDL cholesterol levels, and elevated fasting blood sugar. Metabolic syndrome significantly increases the risk of cardiovascular disease and type 2 diabetes.
Polycystic Ovary Syndrome (PCOS)
PCOS is a hormonal disorder that affects women and is characterized by insulin resistance, hormonal imbalances, and ovarian dysfunction. Insulin resistance plays a significant role in the pathophysiology of PCOS and contributes to its associated symptoms, such as irregular menstrual cycles, infertility, and excessive hair growth. Many women suffering from PCOS go on to develop metabolic syndrome.
The Impact of Diet on Metabolic Function
Diet plays a significant role in metabolic function and can have a profound impact on overall metabolic health. Here are some ways diet influences metabolic function:
Macronutrient balance – The balance of macronutrients, including carbohydrates, proteins, and fats, in the diet can affect metabolic function. The body metabolizes these macronutrients differently, and their consumption can impact insulin sensitivity, glucose regulation, and lipid metabolism and thus lead to metabolic syndrome.
Carbohydrates – Carbohydrates are the primary source of energy for the body. Complex carbohydrates, such as whole grains, legumes, and vegetables, provide fiber and slow-release energy, promoting stable blood sugar levels. On the other hand, consumption of refined carbohydrates and sugars can lead to insulin resistance, weight gain, and an increased risk of metabolic disorders.
The amount of carbohydrates an individual can safely consume to maintain good metabolic health can vary a lot, based on genetic factors, lifestyle habits and hormone balance. A continuous glucose monitor (CGM) can be a valuable tool to determine the optimal carbohydrate intake for each individual.
Proteins – Protein is essential for various metabolic processes, including the synthesis and repair of tissues, hormone production, and enzyme function. Adequate protein intake supports muscle maintenance and can help regulate appetite, promote satiety and contribute to insulin sensitivity.
Fats – Healthy fats, such as monounsaturated fats found in olives, avocados, and nuts, and polyunsaturated omega-3 fats found in fatty fish, seeds, and some nuts are important for metabolic health. They provide essential fatty acids that help support hormone production, cell membrane integrity, and absorption of fat-soluble vitamins.
Fiber – Dietary fiber, found in fruits, vegetables, whole grains, legumes, and nuts, plays a crucial role in metabolic health. It promotes satiety, helps regulate blood sugar levels, supports healthy gut bacteria, and aids in maintaining a healthy body weight.
Hydration – Proper hydration is essential for optimal metabolic function. Water is involved in many metabolic processes, including nutrient absorption, waste removal, and thermoregulation.
Key Nutrients and Their Role in Supporting Metabolic Health:
Several key nutrients play important roles in supporting metabolic health. Here are some examples:
Chromium – Chromium is involved in insulin signaling and glucose metabolism. It helps enhance insulin sensitivity and supports proper glucose utilization. Food sources of chromium include broccoli, barley, green beans, and grape juice.
Magnesium – Magnesium is essential for over 300 enzymatic reactions in the body, including those related to glucose metabolism and insulin action. Adequate magnesium intake supports insulin sensitivity and helps regulate blood sugar levels. Good sources of magnesium include green leafy vegetables, nuts, seeds, and whole grains.
Omega-3 fatty acids – Omega-3 fatty acids, particularly eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), have anti-inflammatory properties and can support insulin sensitivity. They are found in fatty fish like salmon, mackerel, and sardines. Plant-based sources of omega-3 fatty acids, such as flaxseeds, chia seeds, hemp seeds and walnuts, provide alpha-linolenic acid (ALA), which can be converted to EPA and DHA in the body to a limited extent. Algae and purslane are good plant sources of EPA and DHA.
B vitamins – B vitamins, including thiamine (B1), riboflavin (B2), niacin (B3), pantothenic acid (B5), pyridoxine (B6), biotin (B7), folate (B9), and cobalamin (B12), play vital roles in energy metabolism. They are involved in the conversion of carbohydrates, proteins, and fats into usable energy.
Vitamin D: Vitamin D deficiency has been associated with insulin resistance and an increased risk of metabolic disorders. Adequate vitamin D levels are important for insulin sensitivity and maintaining healthy blood sugar levels. Vitamin D can be obtained from sunlight exposure and dietary sources like fatty fish and mushrooms that have been exposed to sunlight.
Antioxidants – Antioxidants, such as vitamins C and E, beta-carotene, and selenium, help protect cells from oxidative damage caused by free radicals. Oxidative stress and inflammation can contribute to metabolic dysfunction. Including a variety of fruits, vegetables, nuts, seeds, and whole grains in the diet can provide a range of antioxidants.
Our on-demand workshop, The Metabolic Recovery Formulas, provides details about insulin resistance and metabolic health.
The Gut Microbiome and Its Influence on Metabolic Health
The gut microbiome refers to the complex community of microorganisms, including bacteria, viruses, fungi, and other microbes, residing in the gastrointestinal tract. The gut microbiome plays a crucial role in maintaining overall health, including metabolic health. Here's how the gut microbiome influences metabolic health:
Nutrient metabolism: The gut microbiome helps break down complex carbohydrates, fibers, and other nutrients that our bodies cannot digest on their own. Through fermentation, gut bacteria produce short-chain fatty acids (SCFAs) that serve as an energy source for the body and play a role in regulating metabolism.
Energy extraction and storage: Certain gut microbes have the ability to extract more calories from the diet by breaking down otherwise indigestible fibers and producing additional SCFAs. This can impact energy balance and contribute to weight gain or obesity if energy intake exceeds expenditure.
Regulation of appetite and satiety: The gut microbiome communicates with the brain through various signaling pathways, influencing appetite and satiety. Some gut bacteria produce molecules that can affect hunger-regulating hormones, such as leptin and ghrelin, and impact food cravings and feelings of fullness.
Inflammation and immune function: Imbalances in the gut microbiome can lead to increased intestinal permeability (“leaky gut”) and the release of bacterial components into the bloodstream, triggering systemic inflammation. Chronic inflammation can disrupt metabolic processes, contribute to insulin resistance, and increase the risk of metabolic disorders.
Bile acid metabolism: Gut bacteria play a role in the metabolism of bile acids, which are involved in the digestion and absorption of dietary fats. Alterations in the gut microbiome can impact bile acid metabolism, potentially influencing lipid metabolism and contributing to dyslipidemia.
Gut Dysbiosis and Its Association with Metabolic Dysfunction
Gut dysbiosis refers to an imbalance or disruption in the composition and function of the gut microbiome. It can occur due to various factors, including poor diet, stress, antibiotic use, and certain medical conditions. Gut dysbiosis has been associated with metabolic dysfunction in several ways:
Insulin resistance and glucose regulation: Imbalances in the gut microbiome have been linked to insulin resistance and impaired glucose regulation. Dysbiotic gut bacteria can produce metabolites that interfere with insulin signaling, promote inflammation, and contribute to metabolic disorders such as prediabetes and type 2 diabetes.
Obesity and weight gain: Alterations in the gut microbiome composition have been observed in individuals with obesity. Dysbiotic gut bacteria can influence energy extraction from the diet, promote fat storage, and affect the regulation of appetite and satiety, contributing to weight gain and obesity.
Lipid metabolism and dyslipidemia: Imbalances in the gut microbiome have been associated with changes in lipid metabolism and an increased risk of dyslipidemia. Dysbiotic gut bacteria can impact bile acid metabolism, which can influence the absorption and metabolism of dietary fats, potentially leading to abnormal lipid profiles.
Inflammation and metabolic disorders: Dysbiosis-induced gut inflammation can contribute to systemic inflammation, which is closely linked to the development of metabolic disorders. Chronic inflammation can disrupt insulin signaling, promote insulin resistance, and contribute to the progression of metabolic dysfunction.
Non-alcoholic fatty liver disease (NAFLD): Gut dysbiosis has been implicated in the development and progression of NAFLD, a condition characterized by excessive fat accumulation in the liver. Dysbiotic gut bacteria can promote inflammation, alter gut barrier function, and contribute to the development of liver steatosis and inflammation.
Understanding the relationship between the gut microbiome and metabolic health is an active area of research, and ongoing studies aim to elucidate the specific mechanisms and identify potential therapeutic interventions targeting the gut microbiome to improve metabolic outcomes.

Understanding the Link Between Inflammation and Metabolic Health
Inflammation is a natural response of the immune system to protect the body against harmful stimuli, such as infections or tissue damage. However, chronic low-grade inflammation can have detrimental effects on metabolic health. Here's how inflammation is linked to metabolic dysfunction:
Adipose tissue dysfunction: In obesity, adipose tissue undergoes changes that contribute to chronic inflammation. Enlarged adipocytes release pro-inflammatory cytokines, such as tumor necrosis factor-alpha (TNF-alpha) and interleukin-6 (IL-6), as well as chemokines that attract immune cells. This adipose tissue inflammation is associated with insulin resistance and metabolic abnormalities.
Insulin resistance: Chronic inflammation interferes with insulin signaling, impairing the ability of cells to respond to insulin and take up glucose from the bloodstream. This leads to elevated blood sugar levels and the development of insulin resistance, a hallmark of metabolic disorders such as type 2 diabetes.
Dysregulation of adipokines: Adipose tissue produces various signaling molecules called adipokines. Inflammatory changes in adipose tissue alter the secretion profile of adipokines, such as adiponectin and leptin, which play important roles in insulin sensitivity, energy balance, and inflammation regulation. Dysregulation of adipokines can contribute to metabolic dysfunction.
Systemic inflammation: Inflammatory molecules produced by adipose tissue and immune cells can enter the bloodstream, leading to systemic inflammation. This chronic low-grade inflammation affects various organs and tissues, including the liver, muscles, and blood vessels, contributing to metabolic dysfunction and the development of conditions like cardiovascular disease.
Recognizing the Unique Metabolic Needs of Each Client
To promote optimal metabolic health, it's crucial to recognize that every individual has unique metabolic needs. Factors such as age, sex, body composition, genetic predispositions, and underlying health conditions can influence metabolic function.
By acknowledging these individual differences, healthcare practitioners can develop personalized approaches to metabolic health.
When addressing metabolic health, it's important to assess individual factors that can impact metabolic function. This includes:
1. Genetics: Genetic factors can influence an individual's susceptibility to certain metabolic conditions and their response to specific interventions. Understanding an individual's genetic predispositions can help tailor interventions accordingly.
2. Lifestyle: Lifestyle factors, such as diet, physical activity levels, sleep patterns, stress levels, and tobacco or alcohol use, can significantly impact metabolic health. Assessing these factors provides insights into areas that may need modification to improve metabolic outcomes.
3. Medical history: Past medical conditions, medication use, and previous treatments can have implications for metabolic health. Conditions such as diabetes, polycystic ovary syndrome (PCOS), thyroid disorders, and cardiovascular diseases can influence metabolic function and guide intervention strategies.
Tailoring Interventions and Treatment Plans for Optimal Metabolic Outcomes
Based on the assessment of individual factors, interventions and treatment plans can be tailored for optimal metabolic outcomes. Here are some considerations for individualized approaches:
Diet and nutrition: Customizing dietary recommendations based on an individual's nutritional needs, preferences, and goals is crucial. This may involve adjusting macronutrient ratios, incorporating specific foods or food groups, considering dietary restrictions or allergies, and addressing nutrient deficiencies.
Physical activity and exercise: Designing personalized exercise programs that consider an individual's fitness level, preferences, and any underlying health conditions is important. This may involve a combination of aerobic exercises, strength training, flexibility exercises, and incorporating activities that the individual enjoys and can sustain long-term.
Supplements: Supplements may be necessary to address specific metabolic conditions or deficiencies. The selection and dosage of supplements should be based on individual needs and guided by functional healthcare professionals.
Behavioral and psychological support: Recognizing the psychological and behavioral aspects of metabolic health is essential. Addressing emotional eating patterns, stress management techniques, and providing support for sustainable behavior change can significantly impact long-term metabolic outcomes.
Regular monitoring and follow-up: Regular monitoring of metabolic markers, such as blood glucose levels, lipid profiles, body composition, and other relevant parameters, allows for ongoing assessment of progress and adjustment of interventions as needed. Regular follow-up visits with healthcare practitioners provide opportunities for feedback, education, and guidance.
By recognizing individual metabolic needs, assessing relevant factors, and tailoring interventions and treatment plans, healthcare practitioners can optimize metabolic outcomes and support long-term good metabolic health for each client.
Prioritizing Metabolic Health
As functional practitioners, it is crucial to prioritize metabolic health in client care. By recognizing the interconnectedness of metabolic processes and their impact on overall well-being, you can play a vital role in promoting optimal metabolic health for your clients.
By addressing factors such as insulin resistance, nutrition, gut health, inflammation, and individualized approaches, you can empower your clients to make positive changes and improve their metabolic well-being.
Also, by implementing evidence-based strategies, providing personalized care, and fostering a supportive and empowering environment, you can guide your clients toward improved metabolic health, reduced risk of chronic diseases, and enhanced overall well-being.
Remember that each client is unique, and taking an individualized approach to metabolic health is essential. By understanding their specific needs, considering their lifestyle factors, and tailoring interventions accordingly, you can help your clients achieve optimal metabolic outcomes and support them on their journey toward long-term health and vitality.
For Further Information
The podcast at ReInventHealthcare.com dives deep into metabolic health and other factors that may affect the lives of your clients.

If you want to make a difference and improve our broken healthcare system, be part of the movement and join me in reinventing healthcare at www.INEMethod.com.







0 Comments
Trackbacks/Pingbacks